Negativity Bias and Eating Disorders: How They Sabotage Your Recovery
Introduction
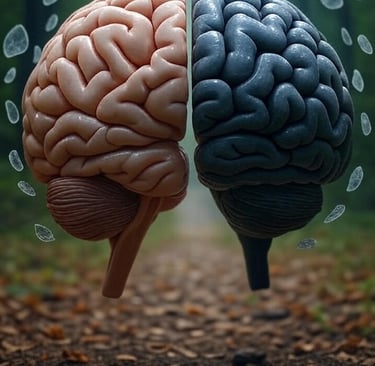
Have you ever wondered why a single negative comment about your appearance can ruin an entire day, even after receiving ten compliments? This phenomenon, called negativity bias, plays a major role in maintaining eating disorders. It creates a vicious cycle where every negative thought feeds problematic behaviors with food and your body image.
This natural tendency of our brain to give more weight to negative experiences than positive ones becomes a real nightmare for people struggling with anorexia nervosa, bulimia, or binge eating disorder. It's like wearing tinted glasses that only let bad news through.
But be careful, we're not talking about simple pessimism or "seeing the glass half empty." These cognitive biases are real brain mechanisms, deeply ingrained, that automatically filter your perception of reality. Understanding them is already taking a big step toward breaking free from their grip.
And here's something important: these thought distortions don't just affect people directly impacted by eating disorders. They also affect families, friends, and even healthcare professionals trying to help. This discovery changes everything about how we approach treatment and support.
Negativity Bias in Eating Disorders: Your Worst Invisible Enemy
Understanding This Mechanism That's Playing Tricks on You
Imagine your brain is equipped with a rigged scale. On one side, positive experiences weigh 1 pound. On the other, negative ones weigh 5 pounds. That's exactly what happens with negativity bias: your mind automatically gives five times more importance to unpleasant events.
In daily life with an eating disorder, this creates exhausting situations. Take Marie's example, in recovery from anorexia: she can receive encouragement all week from loved ones about her progress, but a simple look she interprets as critical will obsess her for days. This look mentally erases all positive moments, as if they never existed.
Your brain isn't broken though! It's a survival mechanism inherited from our ancestors: better to remember the bush where a predator was hiding than the one where berries grew. Except today, this protection system becomes your mental prison, especially when it comes to food and body image.
Brain scans show that in people with eating disorders, the amygdala (your internal danger detector) literally goes into overdrive when faced with food or body-related stimuli. It's like your fire alarm going off for a birthday candle.
How This Bias Sabotages Each Eating Disorder Differently
In anorexia nervosa, negativity bias becomes a true mental tyrant. Every hunger sensation is interpreted as a victory that could be lost, every gram on the scale cancels weeks of therapeutic efforts. It's like trying to fill a leaky bucket: no matter how many positive experiences you pour in, they always end up escaping.
Sarah, 22, describes it this way: "Even when I rationally know I need to eat, my brain turns every bite into a catastrophe. A normal meal becomes proof in my head that I'm losing control of my life."
For bulimia nervosa, this bias creates exhausting emotional roller coasters. A "normal" meal triggers an avalanche of negative thoughts that push toward compensatory restrictions. These restrictions then increase the risk of bulimic episodes. It's a vicious circle where the brain only remembers moments of "loss of control" while completely forgetting all successful balanced meals.
Binge eating disorder sees this mechanism transform into a merciless judge. Every dietary slip, even minor, becomes proof in your head that you're "worthless," "weak-willed," "unable to change." This crushing guilt often pushes people to completely abandon efforts, creating that feeling of helplessness around food that many know all too well.
Other Cognitive Biases: The Organized Gang Maintaining Your Disorder
Selective Attention Bias: Your Mental Blinders
You know the expression "seeing only what you want to see"? In eating disorders, it's more like "seeing only what hurts." Your attention becomes like a spotlight permanently focused on everything related to weight, food, physical appearance.
What does this look like in practice? You enter a room and your gaze automatically fixes on the thinnest person. At a restaurant, you first scan what others are eating before even looking at the menu. In the mirror, your eyes go directly to the area of your body you like least. It's exhausting, but it's automatic.
This constant hypervigilance literally drains your mental energy. It's as if your brain is permanently running a background program that consumes all your resources. No wonder you feel exhausted at the end of the day!
The worst part? While your attention is monopolized by these negative aspects, you completely miss moments of pleasure, sincere compliments, real progress you're making. These positive moments exist, but your brain filters them out like unwanted spam.
Confirmation Bias: Your Personal Devil's Advocate
Imagine having a private detective in your head, but a very bad detective who only looks for evidence confirming your worst fears. That's exactly what confirmation bias does in eating disorders.
You think you're "too fat"? Your brain will meticulously collect all the "evidence": those jeans that are a bit tight (even though they just came out of the dryer), that photo where you don't look your best (out of the 50 where you look great), that ambiguous comment from a colleague (who probably didn't mean any harm).
Meanwhile, all signs that contradict this belief are swept away with a mental backhand. Compliments? "They're just being nice." Clothes that fit well? "It's just a flattering cut." Positive health indicators? "That's not what really matters."
This biased selection of information creates an alternative reality bubble where only negative "evidence" counts. It's like living in a courtroom where only the prosecutor has the right to speak, and the defense attorney is gagged.
Interpretation Distortions: When Everything Becomes an Attack
Your colleague didn't say hello this morning? "They must think I'm fat." Your friend suggests a restaurant? "They think I eat too much." Someone looks at you on the street? "They're judging my appearance." These automatic interpretations transform neutral situations into imaginary aggressions.
It's as if your brain had installed Google Translate, but a defective version that translates everything into hostile language. Silence becomes disapproval, kindness becomes pity, indifference becomes rejection.
These distortions create a parallel reality where you're constantly under attack, judged, criticized. The cruelest part is that these attacks come from your own mind, not from others. You become both the prisoner and the guard of your own mental cell.
How These Biases Sabotage Your Path to Healing
Why It's So Hard to Recognize You Need Help
"I don't really have a problem," "Others have it worse than me," "I can handle this alone"... Do these phrases sound familiar? Denial in eating disorders isn't bad faith, it's your brain protecting you from the distress that would come from fully acknowledging the problem.
Cognitive biases act as a sophisticated defense system. They filter information to maintain consistency with your beliefs, even if these beliefs cause you suffering. It's paradoxical, but your brain prefers familiar suffering to the frightening unknown of change.
For loved ones, this is confusing and frustrating. They clearly see the problem, but the person seems to "refuse" to see it. In reality, their brain is literally showing them another version of reality, filtered by these biases. It's like trying to convince someone wearing red glasses that the world isn't red.
This understanding changes everything in the therapeutic approach. Rather than brutally confronting denial (which often reinforces defenses), it becomes possible to work progressively on the mechanisms that maintain it.
Resistance to Change: When Your Brain Sabotages Your Efforts
You've decided to heal, you're motivated, and yet... Every progress seems insignificant, every relapse becomes the end of the world. It's negativity bias transforming your healing journey into an impossible mountain to climb.
Imagine climbing stairs where each step up seems tiny, but each step down appears huge. That's exactly what your brain does with your progress. This week, you managed 6 normal meals out of 7? Your mind only remembers the failure, not the 6 successes.
Relapses, which are a normal part of any healing process, become definitive proof in your head that "it will never work." It's as if your brain was holding a trial where each relapse is a life sentence, with no possibility of appeal.
This cognitive resistance explains why willpower alone isn't enough. You can have all the motivation in the world, if your brain continues to sabotage your efforts with these biases, it's like trying to swim with an anchor tied to your ankle.
The Impact on Your Loved Ones: When Biases Become Contagious
Your Loved Ones in the Turmoil of Cognitive Distortions
Eating disorders never affect just one person. They create shock waves that affect the entire family and close friends. And guess what? Cognitive biases also become contagious in this context.
Parents often develop their own hypervigilance: they scrutinize every bite, analyze every mood variation, interpret every sign. This constant surveillance, even when well-intentioned, can paradoxically reinforce problematic behaviors by confirming that "eating is dangerous and requires surveillance."
Parental guilt is another bias that sets in: "What did I do wrong?", "If only I had seen the signs earlier"... This guilt creates an atmosphere of tension that can complicate healing, even though it comes from sincere love.
Siblings can develop their own distortions: feeling neglected ("parents only care about them"), fear of developing a disorder themselves, or conversely minimization ("they're exaggerating for attention").
Healthcare Professionals Aren't Immune
Surprise: even experienced therapists can be affected by these cognitive biases! Faced with frequent relapses and slow progress, they can develop a certain therapeutic pessimism, especially if they're not specifically trained in eating disorders.
A professional may unconsciously categorize a patient as "resistant" or "difficult" after a few failures, which influences the quality of care. It's human, but it's problematic. Hence the importance of choosing professionals truly specialized in eating disorders.
Stigmatization also exists in the medical field. Studies show that some professionals still have prejudices about eating disorders, seeing them as "whims" or "rich people's problems." These biases can delay appropriate diagnosis and treatment.
Therapeutic Approaches That Outsmart These Mental Traps
CBT-E: Reprogramming Your Mental Software
Enhanced Cognitive Behavioral Therapy (CBT-E) is like an update program for your brain. Instead of fighting your negative thoughts head-on (which often reinforces them), it teaches you to observe them, understand them, and gradually modify them.
This approach doesn't tell you "stop thinking like that" (if only it were that simple!). Instead, it suggests: "Let's observe together how you think, test if it's really accurate, and see if there are other ways of looking at things."
For example, faced with the thought "If I eat this dessert, I'll gain 2 pounds," CBT-E guides you to examine this belief: Is it biologically possible? What happened the previous times? It's like becoming the Sherlock Holmes of your own thoughts.
The effectiveness of this approach comes from its ability to create lasting changes by modifying both behaviors AND thoughts. It's deep work that takes time, but offers real long-term results.
Cognitive Remediation: Building Your Mental Flexibility
Imagine your brain is a muscle that has developed bad posture habits. Cognitive Remediation Therapy (CRT) is like physical therapy for your mind. It doesn't directly address thoughts about food or body, but works on the basic mechanisms of your thinking.
This approach develops your ability to see situations from different angles, to break out of rigid thought patterns. It's like teaching your brain to do yoga: more flexibility, less rigidity.
The exercises may seem disconnected from the eating disorder at first: puzzles, strategy games, perspective-changing exercises... But they train your brain to be more flexible, more adaptable. This newly acquired flexibility then naturally transfers to your relationship with food and your body.
Patients often appreciate this approach because it's less confrontational. We don't talk directly about weight or food, which reduces anxiety and allows deep work without triggering usual defenses.
Attentional Bias Modification Techniques: Redirecting Your Mental Spotlight
These techniques often use computer programs to retrain your attention to no longer automatically fixate on negative stimuli. It's like teaching your brain to change channels when it lands on a toxic program.
For example, you might do exercises where images appear quickly on screen, and you need to identify the neutral or positive ones among the negative ones. With repetition, your brain gradually learns to no longer automatically prioritize negative stimuli.
The advantage? These changes happen below your consciousness radar. You don't need to "believe" it works or fight against your thoughts. Modifications happen automatically, like a background update.
Practical Tips to Start Outsmarting Your Biases Today
Developing Your Metacognitive Awareness: Becoming the Observer of Your Thoughts
The first step to breaking free from these biases is learning to spot them. Start by becoming a curious observer of your own mind, without judgment. It's like watching clouds pass in the sky: you see them, but you don't have to climb into them.
Practical "Automatic Thoughts Journal" exercise: Each day, note 3 automatic thoughts related to food or your body. No need to analyze, just observe and note. For example:
"I saw someone thin and thought I was huge"
"I ate a cookie and thought I had ruined everything"
"Someone complimented me and I thought they were lying"
After a week, reread. You'll start to see patterns, repetitions. This is the beginning of awareness that allows change.
The "What If It Were a Friend?" Technique
When faced with an automatic negative thought, ask yourself this simple question: "What would I say to my best friend if they had this thought?"
Strangely, we're often much kinder and more rational with others than with ourselves. This technique allows you to access that benevolent wisdom you already have within you.
For example, you think "I ate too much at dinner, I'm worthless." What would you say to a friend in this situation? Probably something like: "One meal doesn't define who you are," "It's normal to eat more some days," "You can regain your balance tomorrow."
The Likelihood Scale: Getting Out of All-or-Nothing
Eating disorders love binary thinking: it's all black or all white, perfect or catastrophic. The likelihood scale introduces shades of gray.
When faced with a catastrophic thought, evaluate its probability from 0 to 100%:
"If I eat this cake, I'll gain 2 pounds" → Really 100% sure? Or more like 5%?
"Everyone is looking at me and judging me" → 100% certain? Or maybe 20%?
This simple evaluation forces your brain out of binary mode and to consider other possibilities. It's like going from black and white TV to color: suddenly, there's a whole spectrum of possibilities between extremes.
The STOP Technique: Your Mental Pause Button
When you feel the negative spiral engaging, use the STOP technique:
S: Stop, physically stop
T: Take a breath, take three deep breaths
O: Observe, observe what's happening inside you without judgment
P: Proceed, continue with a chosen action, not automatic
It's like putting your brain on pause to regain manual control. Instead of letting autopilot take you into negative thoughts, you take back the controls.
Toward Lasting Recovery: Patience and Self-Compassion
Accepting It's a Marathon, Not a Sprint
Reprogramming years of cognitive biases is like learning a new language as an adult. It's possible, but it takes time, practice, and a lot of patience with yourself.
Every small progress counts, even if it seems insignificant. Successfully identifying an automatic thought? Victory! Eating a meal without excessive guilt? Celebration! Accepting a compliment without immediately rejecting it? Champagne (or fruit juice)!
Relapses aren't returns to square one, they're learning opportunities. Your brain is testing the old roads, it's normal. The important thing is to gently return to the new path, without beating yourself up.
The Crucial Importance of Professional Support
Trying to overcome these biases all alone is like trying to see your own blind spots while driving. It's technically impossible without mirrors or someone to guide you.
A professional specialized in eating disorders brings this essential outside perspective. They see patterns you can't see, question assumptions that aren't, and most importantly, they believe in your ability to heal when you no longer believe in it yourself.
Working with a multidisciplinary team (psychiatrist for the medical aspect, psychologist for cognitive work, dietitian-nutritionist for the relationship with food) offers the best chances of success. Each brings their stone to the building of your reconstruction.
Conclusion: Freedom Is at the End of the Path
Negativity bias and other cognitive distortions aren't character flaws or personal weaknesses. They're mechanisms of your brain that can be understood, tamed, and modified. This perspective changes everything: you're not "broken," you just need a software update.
The road to eating disorder recovery is winding, with difficult climbs and sometimes unexpected detours. But every step, even small, brings you closer to freedom. Every time you identify a bias, every time you question an automatic thought, you regain a little power over your life.
Remember: these mechanisms that make you suffer today may have had a protective function at some point in your life. Understanding them with compassion rather than fighting them with violence is already an act of healing.
If you recognize these mechanisms in your daily life, if this reading has resonated with your experience, that's already a huge first step. Simply knowing that these biases exist diminishes their power over you. And if you feel you need help to continue this journey, don't hesitate to ask for it. It's an act of courage, not weakness.
Life without the distorting filter of these biases is possible. A peaceful relationship with food and your body is within reach. The path exists, and you don't have to walk it alone.
"Living and eating are two sides of the same coin - Lighten your relationship with food and free yourself from what doesn't serve you!"
Alexis Alliel - Dietitian-Nutritionist specialized in eating disorders 📧 contact@alexis-alliel-dn.fr | 📱 In-office and video consultations
📚 Recovery Progress: Discover if recovery is possible after 10 years and explore links with psychotrauma. Our article on toxic self-relationship may help.
📚 SCIENTIFIC REFERENCES
To delve deeper into the subject, here are the scientific reference sources on cognitive biases in eating disorders:
Williamson, D. A., Muller, S. L., Reas, D. L., & Thaw, J. M. (1999). "Cognitive Bias in Eating Disorders: Implications for Theory and Treatment." Behavior Modification, 23(4), 556-577. Fundamental study on cognitive mechanisms in eating disorders.
Dobson, K. S., & Dozois, D. J. (2004). "Attentional biases in eating disorders: A meta-analytic review of Stroop performance." Clinical Psychology Review, 24(8), 1001-1022. Meta-analysis on attentional biases.
Brooks, S., Prince, A., Stahl, D., Campbell, I. C., & Treasure, J. (2011). "A systematic review and meta-analysis of cognitive bias to food stimuli in people with disordered eating behaviour." Clinical Psychology Review, 31(1), 37-51.
Puhl, R. M., Latner, J. D., King, K. M., & Luedicke, J. (2014). "Weight bias among professionals treating eating disorders: Attitudes about treatment and perceived patient outcomes." International Journal of Eating Disorders, 47(1), 65-75.
Dahlenburg, S. C., Gleaves, D. H., & Hutchinson, A. D. (2019). "Cognitive remediation therapy for eating disorders: A systematic review." Journal of Eating Disorders, 7, Article 41.
Cooper, Z., & Fairburn, C. G. (2021). "Cognitive Behavioral Therapy for Eating Disorders." Annual Review of Clinical Psychology, 17, 233-257. Updated review on CBT effectiveness in eating disorders.
Baudinet, J., Eisler, I., Simic, M., & Schmidt, U. (2024). "Enhanced cognitive behaviour therapy for adolescents with eating disorders: Development, effectiveness, and future challenges." BioPsychoSocial Medicine, 18, Article 10.

Vivre et manger sont les deux faces de la même pièce
Lighten your relationship with food and free yourself from what hinders you!
+33 6 22 41 55 21
© 2024. All rights reserved.
RPPS : 10007258733
N° ADELI : 75 95 0878 1
